White-Coat Tug-of-War: U.S. Conditions, China’s Model, and the Future of African Health
Executive Summary
Sovereignty for Sale? How Tied Aid and Competing Health Models Are Rewriting Africa’s Pandemic Playbook
American health aid to Africa is being fundamentally restructured.
Traditional grant-based assistance is giving way to performance-driven, co-investment models that rely heavily on private firms, advanced technology, and measurable outcomes.
While these arrangements promise efficiency and accountability, they also impose new fiscal, political, and strategic constraints on recipient countries.
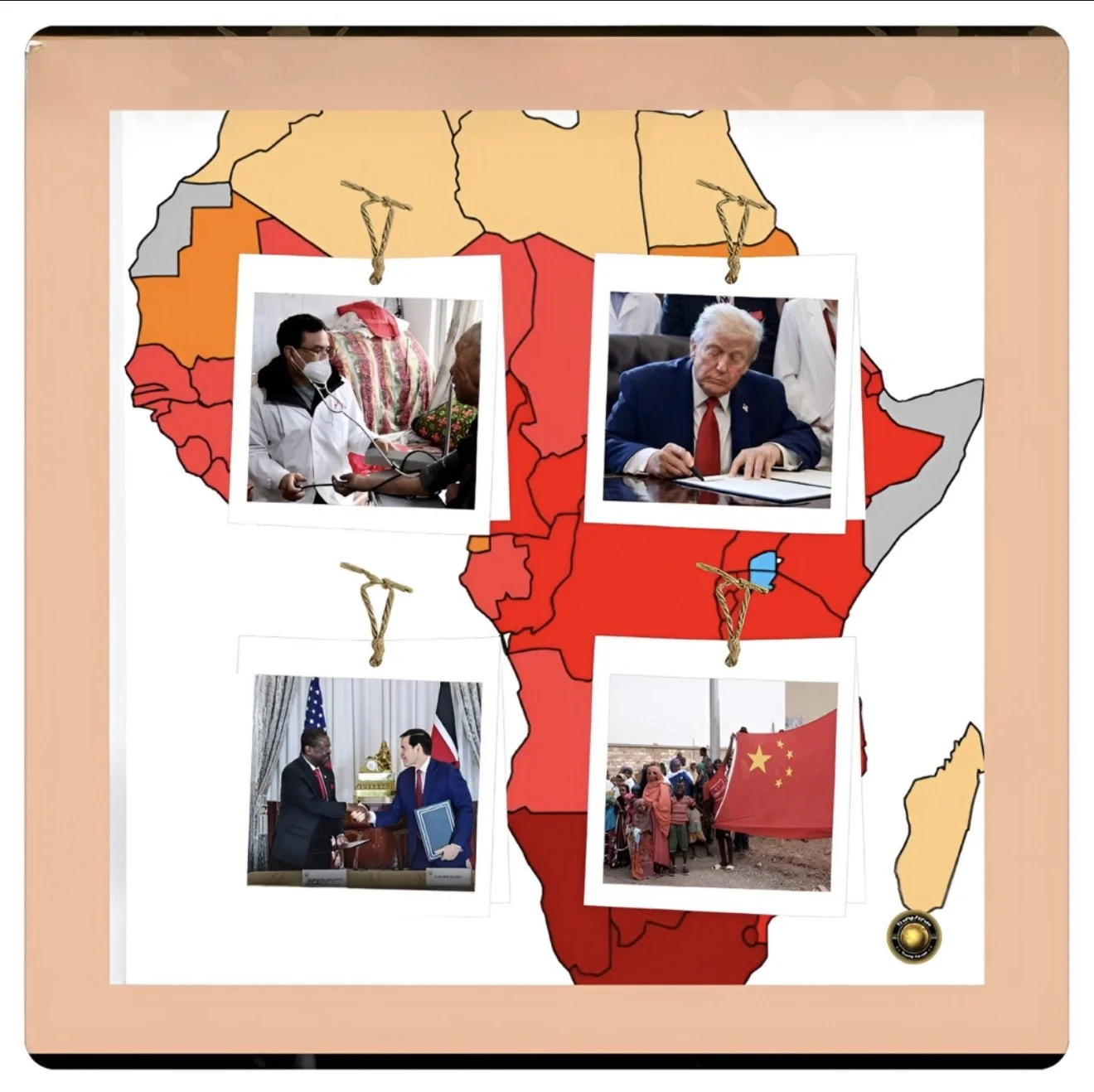
When contrasted with China’s state-led, infrastructure-focused approach to health engagement in Africa, the shift reveals a deeper geopolitical contest over influence, legitimacy, and security.
FAF argues that although the US model delivers speed and innovation, it risks weakening long-term health resilience and policy autonomy if it fails to integrate institutional strengthening.
In a world where health systems are now instruments of national and geopolitical security, the structure of aid matters as much as its scale.
Introduction
From Lifeline to Leverage: How American Health Aid Became a Geopolitical Bargaining Chip in Africa
A drone gliding over a rural clinic in West Africa, releasing blood supplies ordered moments earlier via WhatsApp, captures the promise of a new era of American aid.
Technology replaces trucks, private firms replace public agencies, and contracts replace open-ended commitments. Supporters see reform. Critics see risk.
This transformation comes at a moment when health has moved from the margins of development policy to the center of geopolitics.
Pandemics, demographic pressures, and climate shocks have reframed health systems as pillars of national security.
Against this backdrop, how aid is delivered shapes not only lives saved but political alignment and strategic trust.
History and Current Status
For decades, US health aid to Africa focused on expanding access to essential services through grants, multilateral coordination, and public-sector delivery.
Programs addressing HIV/AIDS, malaria, tuberculosis, and maternal health strengthened ministries, trained workers, and embedded long-term partnerships. The model was imperfect, but it emphasized system-wide capacity.
China’s health engagement followed a different trajectory.
From medical teams and hospital construction to pharmaceutical supply, Beijing emphasized visible steps to build capacity and bilateral relationships.
Health projects were often embedded in broader economic and diplomatic frameworks, reinforcing government-to-government ties.
Today, the United States is recalibrating. Aid increasingly flows through performance-based contracts requiring recipient governments to co-invest financially.
Private companies deliver services, and success is measured through narrow indicators. China, meanwhile, has expanded its health footprint as part of a broader development and security agenda, particularly after the pandemic highlighted the political value of health assistance.
Key Developments
The expansion of drone-based medical logistics illustrates the new American approach. Firms operating across Ghana, Ivory Coast, Kenya, Nigeria, and Rwanda now serve thousands of clinics, supported by aid agreements worth more than $150 million.
These deals require domestic co-financing and guarantee long-term service payments.
In Ghana, rapid blood delivery has reduced delays in emergency care, especially in rural areas where poor roads once proved fatal. Yet officials within the health ministry privately acknowledge the trade-offs.
Annual payments to service providers compete with budgets for training midwives, maintaining facilities, and expanding preventive care. Speed has improved, but systemic depth remains fragile.
Rwanda demonstrates the upside of the model. Strong central coordination and disciplined fiscal planning allow performance-based aid to integrate smoothly into national priorities. Drone logistics complement, rather than distort, broader health strategies.
Chinese-supported hospital upgrades and training programs coexist with American technology, reinforcing capacity rather than fragmenting it. Rwanda’s success, however, highlights a critical limitation: conditional aid works best where institutions are already strong.
Latest Facts and Concerns
Nigeria reveals the risks at scale. While drone services operate efficiently in selected regions, co-investment requirements strain state-level budgets already burdened by salaries and infrastructure deficits.
Chinese-built hospitals appeal to federal ambitions but struggle to compensate for fragmented governance. The result is a patchwork health system shaped as much by donor logic as by national planning.
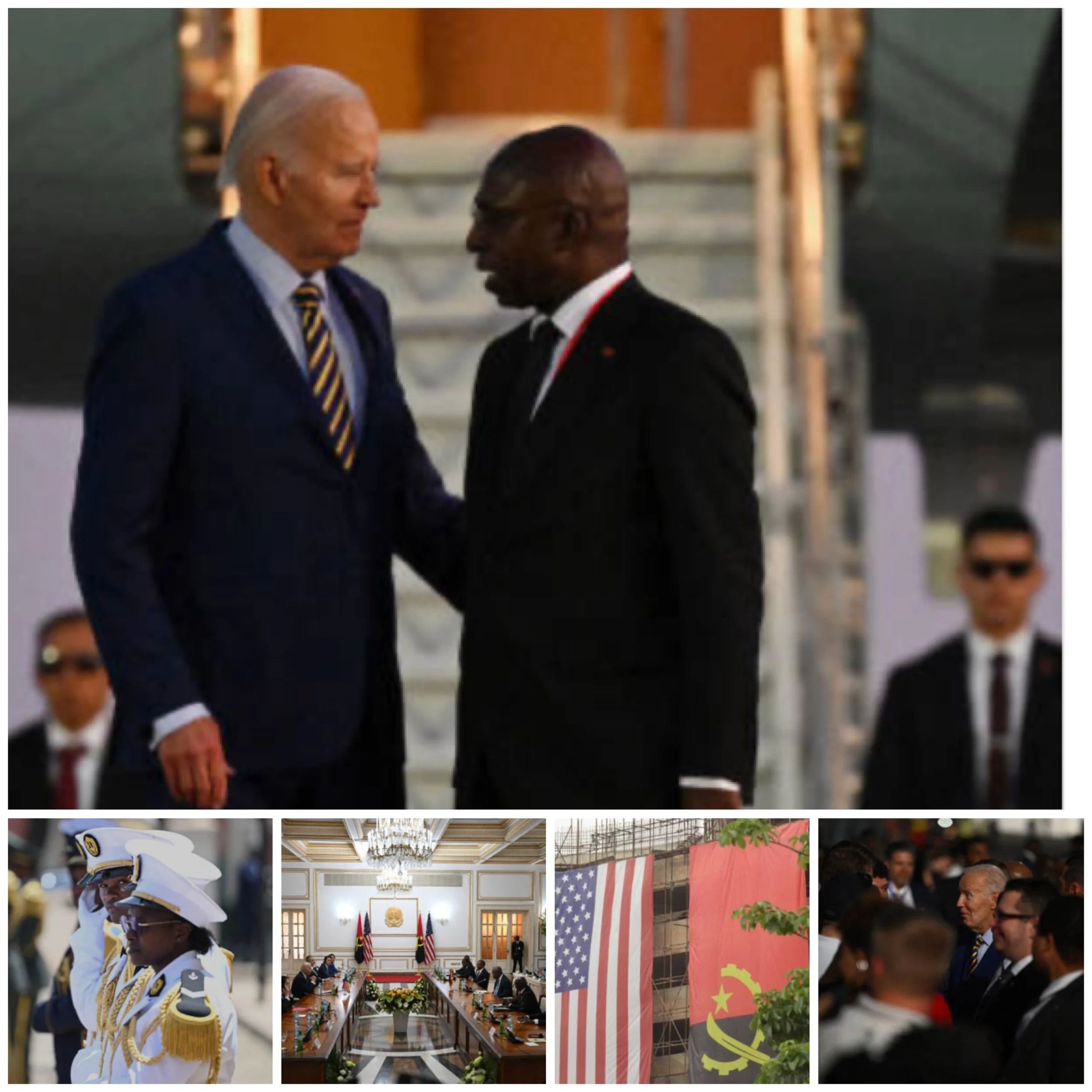
Kenya has adopted a more explicitly strategic posture. American-backed logistics and data systems enhance efficiency, while Chinese-built facilities expand urban care capacity.
Kenyan officials view health aid through a geopolitical lens, deliberately diversifying partnerships to preserve autonomy. Health security, in this context, is inseparable from foreign policy.
Across cases, concerns persist that technology-heavy solutions risk crowding out investments in workforce development, governance, and maintenance.
During health emergencies, drones cannot compensate for shortages of nurses, unreliable electricity, or weak surveillance systems.
Cause-and-Effect Analysis
Conditional aid reshapes incentives. Co-investment requirements privilege fiscally stronger states and urban centers, potentially widening internal inequalities.
Performance metrics favor interventions that are easily quantified, sidelining long-term resilience.
Geopolitically, the US model signals partnership through markets and contracts, while China signals partnership through state capacity and permanence.
African governments respond pragmatically, blending approaches to reduce dependence on any single partner.
The effect is a fragmented health landscape where innovation accelerates delivery but may undermine coherence if not carefully integrated.
Health Security and Geopolitics
Health systems now underpin political legitimacy and crisis response. Countries remember who helped them during emergencies and how.
China’s pandemic-era provision of equipment and vaccines reinforced its image as a dependable partner, even as questions emerged about quality and transparency.
American aid, while technologically impressive, can appear transactional if it prioritizes efficiency over solidarity.
Strategic competition in Africa will not be won by speed alone. Trust, continuity, and alignment with national priorities determine influence.
Future Steps
For American health aid to strengthen both development outcomes and strategic standing, it must integrate innovation with institution-building.
Co-investment terms should be flexible, technology contracts should include training and transfer, and health security should be defined beyond logistics.
Engagement that respects African agency will endure longer than models driven primarily by donor metrics.
Conclusion
China’s Clinics vs. America’s Contracts: The Battle for Africa’s Health Security
American aid to Africa is becoming more conditional, more commercial, and more strategic. In an era of geopolitical rivalry, health security is a form of power.
The contest with China in African health systems will not be decided by drones or hospitals alone, but by whose partnerships strengthen resilience when crises arrive.